Understanding medical conditions can be confusing, but it’s crucial for your health. Vasculitis is one of those less-talked-about conditions that affect blood flow and overall health. Here are ten essential pieces of information about vasculitis to help you grasp its basic concepts and see why early understanding and detection are key.
Understanding Vasculitis and Its Impact
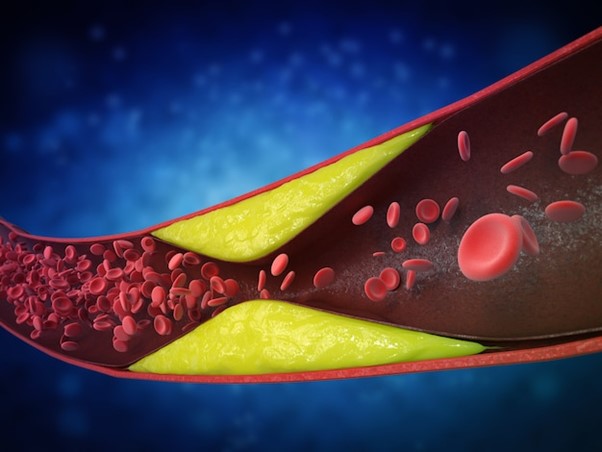
Vasculitis is a medical condition involving the inflammation of vessels – specifically your blood vessels. When these vessels get inflamed, it can disrupt the normal flow of blood through your veins or arteries. This can seriously affect your organs, as they rely on steady blood flow to function properly.
One interesting thing about vasculitis is its variability. This condition doesn’t play favorites; it can affect blood vessels of any size, anywhere in your body. Whether it’s a small capillary in your skin or a large artery near your heart, any vessel can be a target. Because of this, symptoms can range widely from person to person.
The etiology of vasculitis, or its causes, often remains a bit of a mystery. While many cases pop up without a known culprit, certain factors are believed to trigger it. Infections, certain kinds of medications that cause vasculitis, and even toxins from the environment are known to play a part. Not always knowing the direct cause can make treating this condition a bit tricky.
In essence, vasculitis can appear and cause problems in unexpected places. It’s like a silent threat to your blood vessels that can impact your health in myriad ways, demanding awareness and careful monitoring.
Recognizing Symptoms and Challenges in Diagnosis
Spotting the symptoms of vasculitis is vital for early intervention. Common signs include fever and fatigue. These symptoms are quite general and can seem like many things, but they shouldn’t be ignored.
The trickery of vasculitis lies in symptom variety. Since it can affect any organ, its manifestations are equally diverse. If it targets your skin, you might see rashes. If it impacts your nerves, you might feel numbness or tinglings. Trouble breathing? It might be affecting your lungs.
Pinpointing this condition is no walk in the park. Diagnosing vasculitis often requires a blend of tests. A doctor might order blood tests, or look for signs in your blood vessels using imaging. Sometimes, a closer look is needed, and a tissue biopsy can provide the necessary clues. These steps prove that while vasculitis is elusive, it can’t hide forever.
In conclusion, recognizing vasculitis is about paying attention to new or unusual symptoms. This makes the role of medical professionals essential, as they have the tools and knowledge to uncover the issues lurking behind your symptoms.
Types, Causes, and Risk Factors of Vasculitis
Vasculitis isn’t just one-size-fits-all. It’s actually a collection of different types that can affect various vessels and organs. Some target smaller vessels, others go for the larger ones. This means treatment will depend a lot on which vessel it’s targeting.
The root of vasculitis is often tied to your immune system. Most commonly, this condition involves an abnormal immune response. Sometimes, vasculitis presents itself as an autoimmune disease, where the body mistakenly attacks its own blood vessels.
There are several triggers and risk factors for vasculitis. Certain infections might rile up your immune system, leading to blood vessel inflammation. Some specific medications that cause vasculitis are known to trigger this adverse response as well.
Understanding these causes and risk factors is about identifying what might place someone in the crosshairs of vasculitis. It’s about knowing what to avoid and being aware of the changes within your body that warrant a closer look.
Effective Management and the Importance of Early Detection
Don’t be overly alarmed, but do take vasculitis seriously. It’s a rare condition but can be severe, affecting your health significantly if not addressed promptly.
Managing vasculitis effectively involves treatment with specific medications. Corticosteroids can help calm inflammation; immune-suppressing drugs might slow down your immune system’s overzealous attacks on your blood vessels. Getting the right treatment can make all the difference.
If you ever notice symptoms that seem off or don’t go away, seek medical attention. Early detection isn’t just a buzzword here; it’s a way to ensure the management of vasculitis can begin before severe damage takes root.
In summary, vasculitis calls for awareness and diligence. By catching the signs early and seeking medical evaluation, you can make informed decisions that protect your health from the sometimes-devastating impacts of this sneaky condition.